Table of Contents
Sedatives and Hypnotics
Sedation → calming effect without sleep
Hypnosis → induction and maintenance of sleep
Anxiolysis → reduction of anxiety
All classical sedative-hypnotics primarily enhance the action of GABA (Gamma Amino Butyric Acid), the main inhibitory neurotransmitter in the brain.
Neurophysiology Behind Sedation and Sleep
Normal sleep is regulated by:
- Reticular activating system
- Hypothalamus
- Suprachiasmatic nucleus
- GABAergic neurons
Sleep Architecture
Sleep consists of:
NREM (75–80%)
- Stage 1 → light sleep
- Stage 2 → sleep spindles
- Stage 3 → deep restorative sleep
REM (20–25%)
- Dream sleep
- Muscle atonia
- Memory consolidation
Important:
Benzodiazepines decrease REM sleep slightly but less than barbiturates.
Classification of Sedative-Hypnotics
A. Benzodiazepines (Most Common)
Short Acting
- Midazolam
- Triazolam
Intermediate Acting
- Lorazepam
- Alprazolam
Long Acting
- Diazepam
- Clonazepam
B. Barbiturates (Older Drugs)
Ultra Short Acting
Thiopental (IV anesthesia)
Long Acting
Phenobarbital (epilepsy)
C. Non-Benzodiazepine Hypnotics (Z-Drugs)
- Zolpidem
- Zopiclone
- Eszopiclone
Selective for sleep induction.
D. Melatonin Receptor Agonists
Ramelteon
Acts on MT1 & MT2 receptors.
Mechanism of Action
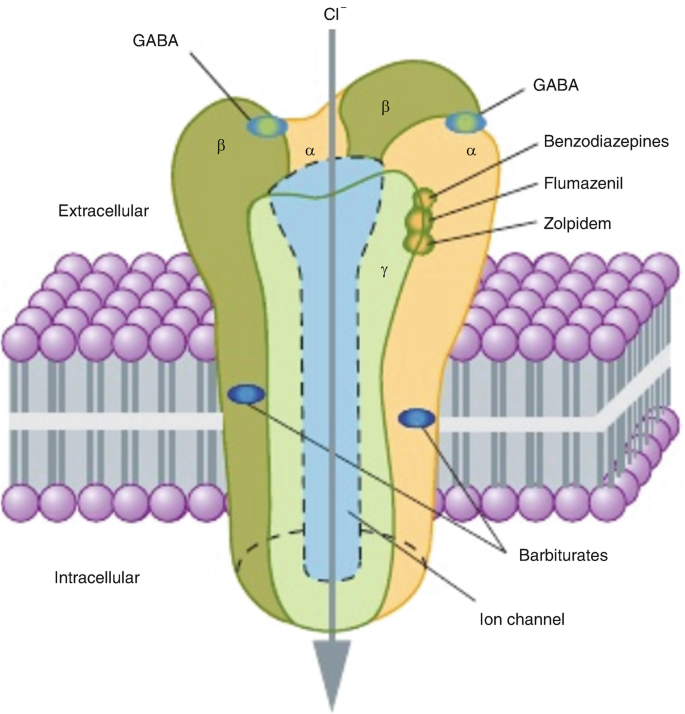
Benzodiazepines
- Bind to benzodiazepine site on GABA-A receptor
- Increase frequency of chloride channel opening
- Require presence of GABA (cannot activate alone)
Result:
⬇ Neuronal firing
⬇ Anxiety
⬇ Muscle tone
⬇ Seizure activity
Barbiturates
- Increase duration of chloride channel opening
- At high doses → directly open channel without GABA
- Narrow therapeutic index
High overdose risk.
Z-Drugs
- Selectively bind α1 subunit of GABA-A receptor
- Mainly produce hypnotic effect
- Minimal muscle relaxant effect
Pharmacokinetics
Absorption
- Well absorbed orally
- Highly lipid soluble
Distribution
- Cross blood-brain barrier rapidly
- Cross placenta
- Present in breast milk
Metabolism
- Liver metabolism (CYP450 enzymes)
- Diazepam forms active metabolites
- Lorazepam does NOT form active metabolites
Elimination
Renal excretion
Elderly patients require dose reduction.
Therapeutic Uses
1. Anxiety Disorders
- Generalized anxiety disorder
- Panic disorder
2. Insomnia
Short-term use recommended (2–4 weeks)
3. Pre-Anesthetic Medication
Midazolam causes anterograde amnesia
4. Epilepsy
- Diazepam (status epilepticus)
- Clonazepam (absence seizures)
5. Alcohol Withdrawal
Prevent delirium tremens
6. Muscle Spasm
- Spinal cord injury
- Cerebral palsy
Adverse Effects
CNS Effects
- Drowsiness
- Impaired coordination
- Confusion (elderly)
- Anterograde amnesia
Respiratory Depression
- Especially with alcohol
- More severe with barbiturates
Tolerance
- Due to receptor downregulation
- Dose escalation required
Dependence
Physical and psychological
Withdrawal Symptoms
- Anxiety
- Tremors
- Insomnia
- Seizures (life threatening)
Drug Interactions
- Alcohol → severe respiratory depression
- Opioids → fatal combination
- CYP inhibitors → increase benzodiazepine levels
Overdose Management
Benzodiazepine Overdose
- Usually safe alone
- Flumazenil used cautiously
Barbiturate Overdose
- Severe respiratory depression
- No specific antidote
- Supportive care + ventilation
Special Populations
Elderly
- Increased fall risk
- Confusion
Pregnancy
Risk of fetal CNS depression
Liver Disease
Prefer Lorazepam (no active metabolites)
Summary
Sedatives and hypnotics act primarily through GABA-A receptor modulation to reduce CNS excitability. Benzodiazepines are safer and widely used, whereas barbiturates are limited due to overdose risk. Long-term use requires caution because of tolerance, dependence, and withdrawal risk.