Table of Contents
Drugs for Cardiovascular System
The cardiovascular system maintains tissue perfusion through a balance between cardiac output, vascular resistance, blood volume, and heart rhythm. Most cardiovascular diseases arise when one or more of these determinants becomes dysregulated.
Pharmacologic therapy therefore targets:
- Vascular tone
- Myocardial contractility
- Blood volume
- Cardiac conduction
- Thrombus formation
Understanding where a drug acts within this physiologic framework makes cardiovascular pharmacology logical rather than memorization-based.
I. Antihypertensive Drugs
Reducing Pressure, Protecting Organs
1. ACE Inhibitors
Examples: Enalapril, Lisinopril, Ramipril
These drugs inhibit the conversion of angiotensin I to angiotensin II. Since angiotensin II is a potent vasoconstrictor and stimulates aldosterone secretion, its inhibition leads to vasodilation and reduced sodium retention.
ACE inhibitors are particularly beneficial in diabetic nephropathy and heart failure because they reduce ventricular remodeling and protect renal function. A persistent dry cough may occur due to bradykinin accumulation.
2. Angiotensin Receptor Blockers (ARBs)
Examples: Losartan, Valsartan, Telmisartan
ARBs block angiotensin II receptors directly. Their clinical effects resemble ACE inhibitors but without causing cough, making them useful alternatives.
3. Beta-Adrenergic Blockers
Examples: Metoprolol, Atenolol, Propranolol, Carvedilol
By blocking β1 receptors in the heart, these drugs reduce heart rate and myocardial contractility, thereby lowering cardiac output and blood pressure.
They are especially useful in hypertensive patients with ischemic heart disease or arrhythmias.
4. Calcium Channel Blockers
Examples: Amlodipine, Nifedipine, Verapamil, Diltiazem
These agents inhibit calcium entry into vascular smooth muscle and cardiac cells. Dihydropyridines (e.g., amlodipine) primarily cause vasodilation, while non-dihydropyridines (verapamil, diltiazem) also reduce heart rate.
5. Diuretics
Examples: Hydrochlorothiazide, Furosemide, Spironolactone
Diuretics promote sodium and water excretion, reducing plasma volume and lowering blood pressure. Thiazides are first-line in uncomplicated hypertension, while loop diuretics are used when fluid overload is present.
II. Antianginal Drugs
Restoring Oxygen Balance
1. Nitrates
Examples: Nitroglycerin, Isosorbide dinitrate
Nitrates release nitric oxide, causing venous dilation. This reduces preload and ventricular wall stress, thereby lowering oxygen demand. Sublingual nitroglycerin provides rapid relief in acute attacks.
2. Beta-Blockers
Examples: Metoprolol, Atenolol
By slowing heart rate and decreasing contractility, these drugs reduce myocardial oxygen consumption. They are effective in chronic stable angina.
3. Calcium Channel Blockers
Examples: Amlodipine, Verapamil
These drugs reduce afterload and improve coronary blood flow. They are particularly useful in variant (Prinzmetal) angina.
III. Drugs Used in Heart Failure
Modifying Disease Progression
 Heart failure develops when the heart cannot pump sufficient blood to meet metabolic demands. Neurohormonal activation initially compensates but eventually worsens myocardial stress.
Heart failure develops when the heart cannot pump sufficient blood to meet metabolic demands. Neurohormonal activation initially compensates but eventually worsens myocardial stress.1. ACE Inhibitors / ARBs
Examples: Enalapril, Lisinopril, Losartan
These reduce afterload and inhibit remodeling, improving long-term survival.
2. Beta-Blockers
Examples: Carvedilol, Metoprolol succinate
These reduce sympathetic overactivation and improve ventricular function over time.
3. Diuretics
Examples: Furosemide, Spironolactone
They relieve congestion and edema. Spironolactone also reduces mortality in severe heart failure by blocking aldosterone.
4. Cardiac Glycosides
Example: Digoxin
Digoxin increases myocardial contractility by inhibiting the Na⁺/K⁺ ATPase pump, raising intracellular calcium. It is especially useful in heart failure with atrial fibrillation.
IV. Antiarrhythmic Drugs
Stabilizing Electrical Activity
Arrhythmias result from abnormal impulse formation or conduction.
Class I – Sodium Channel Blockers
Examples: Lidocaine, Procainamide
These slow phase 0 depolarization.
Class II – Beta-Blockers
Examples: Metoprolol, Propranolol
Reduce sympathetic stimulation of the heart.
Class III – Potassium Channel Blockers
Examples: Amiodarone, Sotalol
Prolong repolarization and refractory period.
Class IV – Calcium Channel Blockers
Examples: Verapamil, Diltiazem
Slow conduction through AV node.
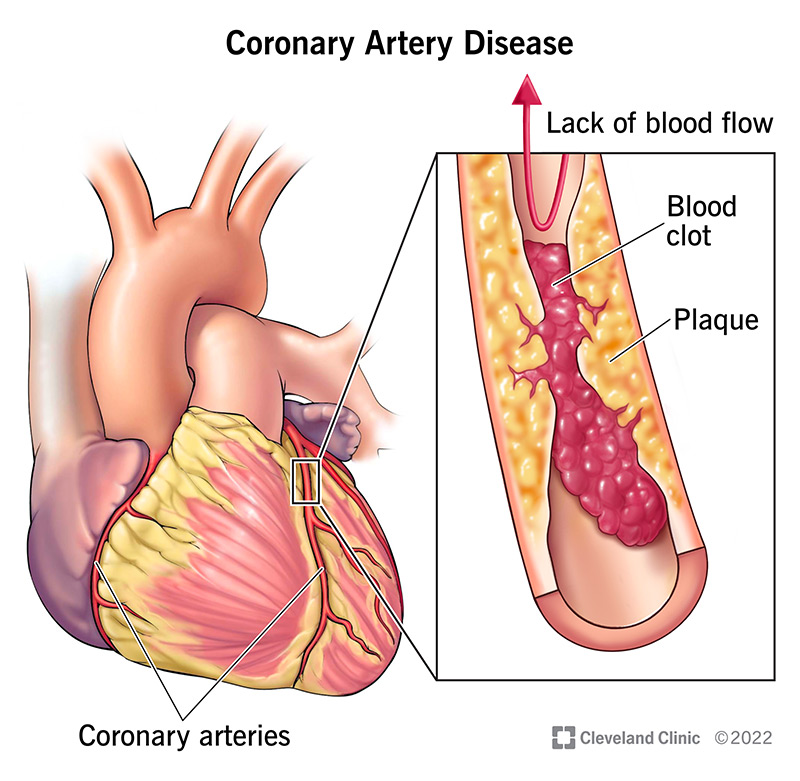
V. Antithrombotic Drugs
Preventing Clot Formation
Antiplatelet Drugs
Examples: Aspirin, Clopidogrel
Aspirin inhibits COX-1 and prevents thromboxane A₂ formation, reducing platelet aggregation.
Anticoagulants
Examples: Heparin, Warfarin, Apixaban
Heparin enhances antithrombin activity, while warfarin inhibits vitamin K-dependent clotting factors. Direct oral anticoagulants like apixaban inhibit factor Xa.
Integrative Perspective
Cardiovascular drugs are not isolated therapeutic tools. Each class modifies fundamental physiologic variables such as preload, afterload, contractility, conduction, or coagulation. Recognizing these relationships allows a deeper conceptual understanding and supports rational prescribing in clinical practice.