Table of Contents
Intraocular Pressure Measurement
INTRAOCULAR PRESSURE
The normal intraocular pressure is 10-20 mm Hg (Schiotz).
Suspicious cases = 20-25 mm Hg (Schiotz).
Glaucoma = above 25 mm Hg (Schiotz).
1. Digital Tension
Principle—The intraocular tension is estimated by palpation of the eyes with fingers.
Method—The patient is asked to look down. The sclera is palpated through the upper lid beyond the tarsal plate. The tension is estimated by the amount of fluctuation.
2. Schiotz Tonometer
Principle—The depth of indentation of the cornea is measured.
Method— The cornea is anaesthetized with suitable local anaesthetic, e.g., xylocaine 4% eyedrops.
- Lids are separated and a tonometer carrying a weight of 5.5 gm is gently placed on the cornea. (There are 3 more weights available 7.5, 10 and 15 gm)
- The deflection is measured and reading in millimeter of mercury can be read from a chart.
Advantages—It is cheap, easy to use, convenient to carry and does not require a slitlamp.
Disadvantage—There may be error due to ocular rigidity.
3. Applanation Tonometer
It is a more accurate method. The cornea is flattened by a plane surface. This is based on the principle of Imbert-Fick’s law. It states that for an ideal, thin-walled sphere, the pressure inside the sphere (P) equals to force necessary to flatten its surface (F) divided by the area of flattening (A), i.e. P = F/A.
Pressure = Force Applied / Area of flattened cornea
P = F / A
An applanation tonometer measures the intraocular pressure by flattening (rather than indent) the cornea over a specific area (3.06 mm). This is more accurate since the pressure values recorded are uninfluenced by scleral rigidity.
Six applanation tonometers are currently in use namely,
- The Goldmann applanation tonometer
- The Perkins tonometer
- The pneumatotonometer
- The air-puff tonometer
- The MacKay-Marg tonometer
- The Microelectronic Tono-pen
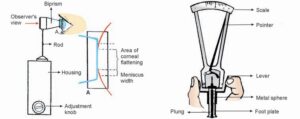
Goldmann applanation tonometer Schiotz tonometer
Goldmann applanation tonometer—It is the most popular and accurate tonometer. It consists of a double prism mounted on a standard slit-lamp. The prism applanates the cornea in an area of 3.06 mm diameter. The normal IOP as measured by applanation tonometer is 15 + 3 Hg.

Method
- Anaesthetise the cornea with a drop of 2% xylocaine and stain the tear film with
- Patient is seated in front of a slit-lamp. The cornea and biprisms are illuminated with cobalt blue light from the slit-lamp.
- Biprism is then advanced until it just touches the apex of the At this point two fluorescent semicircles are viewed through the prism.
- The applanation force against the cornea is adjusted until the inner edges of the two semicircles just touch. This is the end point.
- The intraocular pressure is determined by multiplying the dial reading with
Perkins (hand-held) applanation tonometer—It is same as above except that it does not require a slit- lamp and it can be used even in supine position. It is small and easy to carry.
Pneumatic tonometer—The cornea is applanated by touching its apex by a silastic diaphragm covering the sensing nozzle which is connected to a central chamber containing pressurised air. There is a pneumatic-to-electronic transducer which converts the air pressure to a recording on a paper-strip from where IOP is read.
Air-puff tonometer—It is a non-contact tonometer based on the principle of Goldmann tonometer. The central part of cornea is flattened by a jet of air. This tonometer is very good for mass screening as there is no danger of cross-infection and local anaesthetic is not required.
MacKay-Marg Pulse air tonometer—It is a hand held, non-contact tonometer that can be used on the patients in any position.
Microelectronic Tono-pen—It is a computerised pocket tonometer. It employs a microscopic transducer which applanates the cornea and converts IOP into electrical waves.